INTERNATIONAL MEDICAL JOURNAL
MEDICAL TIPS AND HEALTH SOLUTIONS, RIDWAN UDDIN
Saturday, July 11, 2015
LIPOSUCTION SURGERY
Thursday, February 5, 2015
SEXUAL PROBLEMS WITH SOLUTIOS
How Do I Know If I Have a Sexual Problem?
The most important thing you can do to
determine if you have a sexual problem is to talk honestly and openly
about your symptoms with your health care provider.
Your
health care provider will probably ask about your relationships,
partners, past sexual history, any history of trauma, possible symptoms
of depression, and any other stresses or concerns that may be
interfering with your ability to respond sexually. Though these topics
may seem extraordinarily private, they must be covered to properly
evaluate sexual dysfunction and help you have a more satisfying sex
life.
Your health care provider will give you a thorough physical exam, checking for high blood pressure,
vascular disease, a neurological disorder, or obvious signs of
conditions affecting your penis or testicles. You'll probably be given a
blood test to check for diabetes, thyroid disease, and any other
hormonal disorders your practitioner may suspect. In addition, your
health care provider will review the list of medicatios, and substances you use (including natural remedies) to track whether your sexual dysfunction is connected with them.
Because men normally have multiple erections
during sleep, you'll probably be asked about whether you ever awaken
with an erection. Sometimes men are asked to undergo a test in a sleep
lab to be monitored for erections during sleep. While this information
can help tell whether erectile dysfunction
may be due to problems with the vascular or nervous systems, it doesn't
necessarily indicate whether the erection is sufficient for sexual
penetration. An ultrasound exam that measures the blood flow within the
pelvis (a penile Doppler study) can determine whether there is enough
blood flow and pressure in the penis to allow for an adequate erection.
A measurement of blood pressure in the penis,
called the penile-brachial index, may be helpful in diagnosing penile
vascular disorders. A test dose of an erection-inducing agent, such as
papaverine, is injected into the penis under a doctor's supervision,
followed by monitoring for a subsequent erection. Also, penile blood
pressure can be measured during the erection. During this exam, contrast
dye may also be injected into an artery so X-rays can reveal any leaks
in the vascular system that could account for erectile dysfunction.
What Are the Treatments for Male Sexual Problems?
Any underlying physical conditions will be
treated in an effort to improve your sexual functioning. Medication may
be given to increase testosterone levels, decrease prolactin, treat
thyroid disease, or address high blood pressure. If your sexual
dysfunction seems to be due to medications for another condition, your
health care provider may prescribe an alternative with fewer sexual side
effects. If you smoke, drink alcohol, or use any recreational drugs,
you'll be encouraged to stop. Your health care provider will also
recommend you eat a healthy diet and exercise regularly. Studies have
shown that these measures may slow the buildup of fats that can block
the blood vessels.
Treating Premature Ejaculation
Premature ejaculation is commonly curbed by the
"squeeze" technique, a kind of biofeedback. This method has a high
success rate, and repeated practice usually leads to better natural
control. When you feel that orgasm is imminent, withdraw from your
partner's vagina or anus or signal your partner to stop stimulation. You
(or your partner) then squeezes gently on the head of the penis with
the thumb and forefinger, halting the climax. After 20 or 30 seconds,
begin lovemaking again. Repeat the process if necessary.
Promescent is a drug used to treat premature
ejaculation. The topical spray is applied to the penis and contains
lidocaine, reducing sensitivity and allowing for more ejaculation
control.
Other medications may delay ejaculation, such as
selective serotonin reuptake inhibitors (SSRIs) including Zoloft, Paxil,
and Prozac. None of these drugs is specifically approved by the FDA to
treat premature ejaculation.
Premature ejaculation may signal a more complex disorder, and any psychological aspects should be explored in therapy.
Erectile Dysfunction Treatments
Treatments for erectile dysfunction include any of the following:
- The drugs Viagra, Cialis, Stendra, or Levitra and Staxyn
- A vacuum inflation device that pulls blood into the penis
- Prostaglandin urethral suppositories
- Self-injection of medications directly into the penis
- Vascular surgery to correct problems involving the veins of the penis (note: this procedure has not been found to be effective.)
- Inflatable penile implants
Treating Retarded Ejaculation
This sexual problem is often treated by reducing
anxiety and learning to control the timing of ejaculation. Sensate focus
exercises may help; you should withhold penetration until you sense
that ejaculation is inevitable. A common cause of retarded or delayed
ejaculation is side effects from medication, especially antidepressant
medications such as the SSRIs.
Treating Retrograde Ejaculation
Retrograde
ejaculation may be corrected through medications or surgery that allows
the valve at the base of the bladder to close. This is basically a
harmless disorder, causing a problem only if pregnancy is a goal; in
such situations, it may be possible to retrieve sperm from the bladder
for artificial insemination.
Treating Environmental and Psychological Causes of Sexual Problems
Your health care provider may be able to help you
outline strategies to address non-medical issues. If you have
psychological barriers to sexual functioning, your health care provider
may suggest that you seek individual psychotherapy, couples therapy with
your partner, or consult a sex therapist. A number of techniques and
therapies can help individuals, including those who have experienced
sexual trauma, become more comfortable with their sexuality. Similarly,
if your health care provider feels that you may need more information
about sexual functioning to help you achieve greater enjoyment, you may
be referred to a sex therapist.
Treatment for sexual problems
-
Lack of desire. This increasingly common
problem occurs when people lack any interest in sexual fantasies or
activity and suffer distress or relationship problems as a result.
-
Treatment is a multi-step process. Therapists begin by
helping clients identify negative attitudes about sex, explore the
origins of those ideas and find new ways of thinking about sex. The
focus then shifts to behavior: therapists may ask clients to keep
diaries of their sexual thoughts, watch erotic films or develop
fantasies. Therapists also address any relationship problems.
-
Treatment is a multi-step process. Therapists begin by
helping clients identify negative attitudes about sex, explore the
origins of those ideas and find new ways of thinking about sex. The
focus then shifts to behavior: therapists may ask clients to keep
diaries of their sexual thoughts, watch erotic films or develop
fantasies. Therapists also address any relationship problems.
-
Erectile dysfunction. When the penis fails to become or stay erect, intercourse becomes impossible.
-
The cause is typically a mix of physical and psychological
factors. Physical causes include illnesses like diabetes or medication
side effects. One of the main psychological causes is performance
anxiety. After the first incident, men sometimes get so nervous the
problem occurs again.
-
Therapy focuses on reducing anxiety by taking the focus off
intercourse. For men with physical problems, medication or devices can
help.
-
The cause is typically a mix of physical and psychological
factors. Physical causes include illnesses like diabetes or medication
side effects. One of the main psychological causes is performance
anxiety. After the first incident, men sometimes get so nervous the
problem occurs again.
-
Premature ejaculation. Ejaculation is premature when it occurs so soon after intercourse begins that it causes emotional distress.
-
While the causes still aren't understood, treatment works
in almost all cases. Therapy focuses on behavioral training. With his
partner's help, the man learns to withstand stimulation for longer and
longer periods.
-
While the causes still aren't understood, treatment works
in almost all cases. Therapy focuses on behavioral training. With his
partner's help, the man learns to withstand stimulation for longer and
longer periods.
-
Painful intercourse. Painful intercourse, or
dyspareunia, is recurrent or persistent genital pain that causes
significant distress or relationship problems.
-
Most cases — especially among men — involve a physical
problem. A urologist or gynecologist should rule out or address any
medical concerns. For women, the typical treatment focuses on relaxation
training.
-
Most cases — especially among men — involve a physical
problem. A urologist or gynecologist should rule out or address any
medical concerns. For women, the typical treatment focuses on relaxation
training.
Wednesday, February 4, 2015
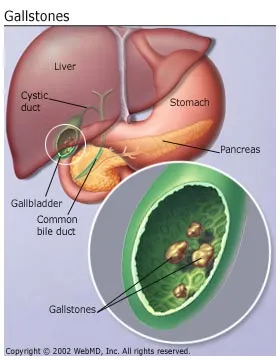
GALL STONE TREATMENT
What Are Gallstones?
Gallstones are pieces of solid material that form in
the gallbladder. These stones develop because cholesterol and pigments
in bile sometimes form hard particles.
The two main types of gallstones are:
- Cholesterol stones: Usually yellow-green in color, approximately 80% of gallstones are cholesterol stones.
- Pigment stones: These stones are smaller and darker and are made up of bilirubin.
What Causes Gallstones?
Several factors may come together to create gallstones, including:
- Genetics
- Body weight
- Decreased motility (movement) of the gallbladder
- Diet
Gallstones can form when there is an imbalance in
the substances that make up bile. For instance, cholesterol stones may
develop as a result of too much cholesterol in the bile. Another cause
may be the inability of the gallbladder to empty properly.
Pigment stones are more common in people with
certain medical conditions, such as cirrhosis (a liver disease in which
scar tissue replaces healthy liver tissue) or blood diseases such as
sickle cell anemia.
What Are the Risk Factors for Gallstones?
Risk factors for getting gallstones include:
- Genetics. If other people in your family have had gallstones, you are at increased risk of developing gallstones.
- Obesity. This is one of the biggest risk factors. Obesity can cause a rise in cholesterol and can also keep the gallbladder from emptying completely.
- Estrogen. Estrogen can increase cholesterol and reduce gallbladder motility. Women who are pregnant or who take birth control pills or hormone replacement therapy have higher levels of estrogen and may be more likely to develop gallstones.
- Ethnic background. Certain ethnic groups, including Native Americans and Mexican-Americans, are more likely to develop gallstones.
- Gender and age. Gallstones are more common among women and older people.
- Cholesterol drugs. Some cholesterol-lowering drugs increase the amount of cholesterol in bile, which may increase the chances of developing cholesterol stones.
- Diabetes. People with diabetes tend to have higher levels of triglycerides (a type of blood fat), which is a risk factor for gallstones.
-
Rapid weight loss. If a person loses weight too quickly,
his or her liver secretes extra cholesterol, which may lead to
gallstones. Also, fasting may cause the gallbladder to contract less.
How Are Gallstones Diagnosed?
If your doctor suspects you have gallstones, he or she will do a physical exam and may perform various other tests, including the following: - Blood tests: Blood tests may be given to check for signs of infection or obstruction and/or to rule out other conditions.
- Ultrasound: This procedure produces images of various parts of the body and can be used to identify gallstones.
- CAT scan: This test uses specialized X-rays to create cross-section images of organs and body tissues.
-
Magnetic resonance cholangiopancreatography (MRCP): This test uses a magnetic field and pulses of radio wave energy to get pictures of structures inside the body, including the liver and the gallbladder.
- Cholescintigraphy (HIDA scan): This test can determine whether the gallbladder is contracting correctly. A radioactive material is injected into the patient and makes its way to the gallbladder. The technician can then observe the movement of the gallbladder.
- Endoscopic ultrasound: This test combines ultrasound and endoscopy to look for gallstones.
- Endoscopic retrograde cholangiopancreatography (ERCP): The doctor inserts an endoscope through the patient's mouth down to the small intestine and injects a dye to allow the bile ducts to be seen. The doctor can often then remove any gallstones that have moved into the ducts.
How Are Gallstones Treated?
Gallstones are usually treated with surgery to take
out the gallbladder. The traditional operation is called an open
cholecystectomy. A newer procedure, called laparoscopic cholecystectomy,
is less invasive, has fewer complications, and is used more often.
- Laparoscopic cholecystectomy. During this procedure, instruments, a light, and a camera are passed through several small incisions in the abdomen. The surgeon views the inside of the body by looking at a video monitor. This procedure is used in of the majority of gallbladder removals. After the surgery, the patient spends the night in the hospital.
- Open cholecystectomy. This is a more invasive procedure in which the surgeon makes incisions in the abdomen to remove the gallbladder. The patient stays in the hospital for a few days after the surgery.
If gallstones are in the bile ducts, endoscopic
retrograde cholangiopancreatography may be used to find and remove them
before or during gallbladder surgery.
Are There Any Nonsurgical Treatments for Gallstones?
If you have a medical condition and your
doctor feels you shouldn't have gallstone surgery, he or she may
prescribe the medications ursodiol (Actigall) and chenodiol (Chenix).
These drugs work by dissolving cholesterol stones. Mild diarrhea can be a
side effect of both medications.
The downside of using either medication is that
you may have to take it for years to completely dissolve the stones. In
addition, the stones may come back after you stop taking the drug.
Sunday, March 31, 2013
TREATMENT OF TYPHOID
Treatments and drug
Antibiotic therapy is the only effective treatment for typhoid fever.Commonly prescribed antibiotics
- Ciprofloxacin (Cipro). In the United States, doctors often prescribe this for nonpregnant adults.
- Ceftriaxone (Rocephin). This injectable antibiotic is an alternative for women who are pregnant and for children who may not be candidates for ciprofloxacin.
Problems with antibiotic resistance
In the past, the drug of choice was chloramphenicol. Doctors no longer commonly use it, however, because of side effects, a high rate of health deterioration after a period of improvement (relapse), and widespread bacterial resistance.
In fact, the existence of antibiotic-resistant bacteria is a growing problem in the treatment of typhoid, especially in the developing world. In recent years, S. typhi also has proved resistant to trimethoprim-sulfamethoxazole and ampicillin.
Supportive therapy
Other treatment steps aimed at managing symptoms include:
- Drinking fluids. This helps prevent the dehydration that results from a prolonged fever and diarrhea. If you're severely dehydrated, you may need to receive fluids through a vein in your arm (intravenously).
- Eating a healthy diet. Nonbulky, high-calorie meals can help replace the nutrients you lose when you're sick.
Throat infection
Medicines and treatments for a throat infection
A sore throat will often get better by itself, as the body’s immune
system can usually take care of the infection without any treatment. Antibiotics aren’t helpful for most people with a throat infection.
Most throat infections are caused by a virus, so antibiotics won’t help. Antibiotics don’t kill viruses.
Even when a throat infection is caused by bacteria, antibiotics are only recommended for people who are more likely to get complications of a throat infection or develop tonsillitis.
There are some simple but effective ways you can relieve your symptoms at home, as well as taking over-the-counter medicines for pain and fever.
Most throat infections are caused by a virus, so antibiotics won’t help. Antibiotics don’t kill viruses.
Even when a throat infection is caused by bacteria, antibiotics are only recommended for people who are more likely to get complications of a throat infection or develop tonsillitis.
There are some simple but effective ways you can relieve your symptoms at home, as well as taking over-the-counter medicines for pain and fever.
Friday, March 15, 2013
ABOUT CONJUNCTIVITIS
What is conjunctivitis

| Inflammation is seen as reddish change in the periphery of the eye often accompanied by a pus-like discharge. |
It usually affects both eyes at the same time – although it may start in one eye and spread to the other after a day or two. It may be asymmetrical, affecting one eye more than the other.
There are many causes and the treatment will depend upon the cause.
Conjunctivitis is a common eye condition. It's not serious, but it can be uncomfortable and irritating.
What causes conjunctivitis
Bacterial conjunctivitis
Bacterial conjunctivitis is an infection caused by bacteria such as staphylococci, streptococci or haemophilus. These organisms may come from the patient's own skin or upper respiratory tract or they may be caught from another person with conjunctivitis.Viral conjunctivitis
Viral conjunctivitis is often associated with the common cold This may be caused by a virus called 'adenovirus'. This type of conjunctivitis can spread rapidly between people and may cause an epidemic of conjunctivitis.Chlamydial conjunctivitis
This type of conjunctivitis is caused by an organism called Chlamydia trachomatis. This organism may also affect other parts of the body and can cause the sexually transmitted infection chlamydiaAllergic conjunctivitis
Allergic conjunctivitis is common in people who have other signs of allergic disease such as hay fever asthma and eczema. The conjunctivitis is often caused by antigens like pollen, dust mites or cosmetics.Reactive conjunctivitis – chemical or irritant conjunctivitis
Some people are susceptible to chemicals in swimming pools or to smoke or fumes, and this can cause an irritation of the conjunctiva with discomfort, redness and watering. In such cases these irritants should be avoided.What are the symptoms of conjunctivitis
Bacterial conjunctivitis
This is a condition that affects both eyes. The eyes will usually feel gritty and irritated with a sticky discharge. The eyelids may be stuck together particularly in the mornings, and there may be discharge or crusting on the eyelashes.Viral conjunctivitis
The eyes are red and there may be a watery discharge.Often the eyelids are very swollen and even the conjunctiva on the white of the eye may be swollen, creating a glassy appearance.
The eyes are uncomfortable, and there may also be the generalised symptoms of a cold. Sometimes there are tender lymph nodes (swollen glands) around the ear or the neck.
This type of conjunctivitis may also spread to affect the cornea (keratitis), and it may persist for several weeks and cause hazy vision.
Chlamydial conjunctivitis
One or both eyes will be red with a sticky discharge and, sometimes, swollen eyelids. The cornea may also be involved in this condition.Allergic conjunctivitis
Allergic conjunctivitis is usually associated with intense itching of the eyes.There may be a stringy discharge and the eyes are usually intermittently red. This may occur at particular times of the year, for instance during spring and summer when there is a lot of pollen in the air.
Conjunctivitis in young children
Small children may be susceptible to infective conjunctivitis, and they may develop severe forms of the condition because of poor immune defences.This is particularly the case in babies, and conjunctivitis in an infant aged less than one month old is a notifiable disease in the UK.
This type of conjunctivitis (ophthalmia neonatorum) may be due to an infection that has been contracted during the passage through the mother’s birth canal and may include the sexually transmitted diseases , such as gonococcal or chlamydial infection.
Small babies may develop conjunctivitis from other types of infection, but swabs should always be taken in order that appropriate treatment can be given.
Small babies often have poorly developed tear drainage passages (a condition known as nasolacrimal duct obstruction).
These children are susceptible to watering eyes and they may intermittently become sticky, but this is usually not serious and most of the time this settles down with no treatment.
How is conjunctivitis treated
Bacterial conjunctivitis
This is usually treated with broad spectrum antibiotic drops or ointment, (eg cholarmphnicol or frusidic acidd).The eyes should also be cleaned with cotton wool soaked in cooled boiled water to remove any crusts or stickiness.
For bacterial conjunctivitis, research evidence shows that while 64 per cent of cases will clear on their own within five days, antibiotic eye medication does lead to increased cure rates and earlier remission.
Viral conjunctivitis
There is no effective treatment for viral conjunctivitis. But the eyes may be made more comfortable by using a lubricant ointment such as lacri lubeCold compresses on the eyes and tablets, such as paracetamol and ibufrofen , can help the symptoms.
As this is a highly contagious condition, it's important to ensure that a strict code of hygiene is adhered to, such as hand and face washing and no sharing of face towels.
Close contact with other people, eg at school, is not recommended for the first one to two weeks to help prevent spread of the infection.
This condition may go on for a prolonged time and in some instances corticosteroid drops have been advocated although these should only be given under the strict supervision of a doctor specialising in eye disease (ophthalmologist).
Chlamydia conjunctivitis
Treatment is with chlorotetracycline ointment to both eyes and tetracycline tablets in order to ensure that infection elsewhere is controlled.Children cannot be treated with tetracycline tablets, and erythromycin is usually used for them.
Because of the possible infection of other mucous membranes any associated sexually transmitted infection should be identified and both the patient and their partners must be treated.
Conjunctivitis in infants
This needs to be taken very seriously.Specimens are taken from the sticky discharge and such children must be seen by an ophthalmologist.
Treatment is given depending on the underlying cause of the conjunctivitis, based on results of the swabs from the laboratory.
Allergic conjunctivitis
This can be treated using topical antihistamine drops.Drops, such as sodium cromoglicate , can be used to prevent the allergic response and they need to be used for many weeks in order to give any result.
Corticosteroid drops are occasionally used, but should only be used under the supervision of an ophthalmologist.
The main treatment should be identifying what is triggering off the allergic response and removing this source of allergen.
What is Trachoma
Trachoma is a form of conjunctivitis that is common in the developing world, particularly in parts of Africa and Asia.It's exacerbated by a lack of clean water because it's spread by contact with other infected people and by flies.
Trachoma is one of the world’s greatest causes of blindness because long-standing infection develops and causes scarring of the eyelids and eyes.
The most effective treatment is to provide a clean supply of water that allows good hygiene.
Antibiotics are also effective in treating the infection in the short term, but recurrent re-infection from within communities causes more damage.
How does the doctor make the diagnosis
Conjunctivitis can usually be diagnosed and treated by your GP.The doctor will usually diagnose the condition based on examination of your eyes and the history that you give.
Sometimes, a swab has to be taken from the eye – especially if there is no improvement on standard treatment.
In some cases that are severe or do not respond to treatment, you may need to see an eye specialist (ophthalmologist).
What should I pay particular attention to?
If there is any worsening of the symptoms despite treatment or if the vision deteriorates, a further consultation with your doctor should be requested even if treatment is being carried out.If you wear contact lenses and develop symptoms of conjunctivitis, it's important to see your doctor. People who wear contact lenses can develop a serious infection of the cornea which requires specialist treatment.
What can be done to avoid conjunctivitis
Good hygiene of hands and face is important. There should be no sharing of face towels, especially if someone has conjunctivitis.Conjunctivitis can spread from one eye to the other, especially when you rub your eyes. Pus and crust should be removed by bathing the eye with lukewarm salt water, which can also lessen the symptoms.
Use disposable tissues when you dry the eyes and throw them away after use. This will limit the contamination. Dispose of any antibiotic eye drops after the treatment is over.
People who suffer from conjunctivitis should have a special towel that only they use.
It is sensible to never share eye make up or eye drops with another person.
How does conjunctivitis usually progress
Even if left untreated, most forms of conjunctivitis will gradually get better on their own in a few weeks. Allergic conjunctivitis usually continues while there's exposure to the aggravating agent.With appropriate treatment, the eyes are usually more comfortable within a few days, although cases of adenoviral infection may cause problems for some weeks.
Thursday, March 14, 2013
ABOUT SEXUALLY TRANSMITED DISEASES
Don't try to treat a sexually transmitted disease, or STD, yourself.
These diseases are contagious and serious. You must see a doctor.
Bacterial STDs can be cured with antibiotics if treatment begins early enough. Viral STDs cannot be cured, but you can manage symptoms with medications. There is a vaccine against hepatitis B, but it will not help if you already have the disease.
If you are given antibiotics to treat a STD, it is important that
you take all of the drug prescribed to you, even if the symptoms go
away. Also, do not take someone else's medication to treat your
infection; it may make it more difficult to treat..
Here are some specific STD treatments:
HIV/AIDS: Since AIDS is not curable, treatment focuses on keeping HIV levels in check. Antiretroviral drugs are the standard therapy for HIV infection, and usually you will be given several drugs to take, a so-called drug "cocktail." The question of when to begin antiretroviral therapy for HIV is still debated. Some doctors believe in an early start to better manage the HIV virus, while others believe it is better to wait since the drugs can cause unpleasant side effects and drug resistance may develop. Talk to your doctor about when you should begin antiretroviral therapy.
Chlamydia and Gonorrhea: These STDs are treated with antibiotics. You should begin taking them if tests show you have chlamydia or gonorrhea or if you have been exposed to them, even though you may not have symptoms. Your sex partners will also have to be treated regardless of whether they have symptoms. Certain strains of gonorrhea have become resistant to some antibiotics, so you may have to take more than one drug to fight gonorrhea. Failure to treat chlamydia or gonorrhea can result in permanent damage to your reproductive organs and an inability to get pregnant.
Syphilis: Penicillin is the preferred treatment for syphilis. Early treatment is crucial to prevent the bacteria from spreading to and damaging other organs.
GENITAL HERPES Once you are infected with genital herpes, the virus remains in your body for life. After the first outbreak, herpes may flare up several times per year, but these episodes may lessen over time. Antiviral medication (such as Zovirax, Famvir, and Valtrex) can help reduce the length and severity of both the initial and subsequent herpes outbreaks. If you have outbreaks often, you may want to use suppressive therapy. In suppressive therapy, your doctor prescribes medicine for you to take every day, to prevent you from getting a herpes outbreak.
GENITAL WARTS : There is no standard of treatment for genital warts. Most genital warts will disappear without treatment, so your doctor may choose to do nothing. However, you will still carry the virus that causes warts and can still transmit it to sex partners. If you do choose to treat genital warts, you have several options. Freezing the warts or applying medication directly to them are often the first choices. If genital warts do not respond to these options, surgery may be necessary to remove them. Keep in mind that treatment does not rid you of the infection, and you can still transmit it to others.
Bacterial STDs can be cured with antibiotics if treatment begins early enough. Viral STDs cannot be cured, but you can manage symptoms with medications. There is a vaccine against hepatitis B, but it will not help if you already have the disease.
Recommended Related to Sexual Conditions
Trichomoniasis >>> is a sexually transmitted disease (STD)
caused by a small organism called Trichomonas vaginalis. Women are most
often affected by this disease, although men can become infected and
pass the infection to their partners through sexual contact.
Here are some specific STD treatments:
HIV/AIDS: Since AIDS is not curable, treatment focuses on keeping HIV levels in check. Antiretroviral drugs are the standard therapy for HIV infection, and usually you will be given several drugs to take, a so-called drug "cocktail." The question of when to begin antiretroviral therapy for HIV is still debated. Some doctors believe in an early start to better manage the HIV virus, while others believe it is better to wait since the drugs can cause unpleasant side effects and drug resistance may develop. Talk to your doctor about when you should begin antiretroviral therapy.
Chlamydia and Gonorrhea: These STDs are treated with antibiotics. You should begin taking them if tests show you have chlamydia or gonorrhea or if you have been exposed to them, even though you may not have symptoms. Your sex partners will also have to be treated regardless of whether they have symptoms. Certain strains of gonorrhea have become resistant to some antibiotics, so you may have to take more than one drug to fight gonorrhea. Failure to treat chlamydia or gonorrhea can result in permanent damage to your reproductive organs and an inability to get pregnant.
Syphilis: Penicillin is the preferred treatment for syphilis. Early treatment is crucial to prevent the bacteria from spreading to and damaging other organs.
GENITAL HERPES Once you are infected with genital herpes, the virus remains in your body for life. After the first outbreak, herpes may flare up several times per year, but these episodes may lessen over time. Antiviral medication (such as Zovirax, Famvir, and Valtrex) can help reduce the length and severity of both the initial and subsequent herpes outbreaks. If you have outbreaks often, you may want to use suppressive therapy. In suppressive therapy, your doctor prescribes medicine for you to take every day, to prevent you from getting a herpes outbreak.
GENITAL WARTS : There is no standard of treatment for genital warts. Most genital warts will disappear without treatment, so your doctor may choose to do nothing. However, you will still carry the virus that causes warts and can still transmit it to sex partners. If you do choose to treat genital warts, you have several options. Freezing the warts or applying medication directly to them are often the first choices. If genital warts do not respond to these options, surgery may be necessary to remove them. Keep in mind that treatment does not rid you of the infection, and you can still transmit it to others.
Wednesday, March 13, 2013
TREATMENT OF SEXUAL ADDICTION
The term " sexual addiction" is used to describe the behavior of
a person who has an unusually intense sex drive or an obsession with sex. Sex
and the thought of sex tend to dominate the sex addict's thinking, making it
difficult to work or engage in healthy personal relationships.
Sex addicts engage in distorted thinking, often rationalizing and justifying their behavior and blaming others for problems. They generally deny they have a problem and make excuses for their actions.
Sexual addiction also is associated with risk-taking. A person with a sex addiction engages in various forms of sexual activity, despite the potential for negative and/or dangerous consequences. In addition to damaging the addict's relationships and interfering with his or her work and social life, a sexual addiction also puts the person at risk for emotional and physical injury.
For some people, the sex addiction progresses to involve illegal activities, such as exibitionism (exposing oneself in public), making obscene phone calls, or molestation. However, it should be noted that sex addicts do not necessarily become sex offenders.
Behaviors associated with sexual addiction include:
Most sex addicts live in denial of their addiction, and
treating an addiction is dependent on the person accepting and admitting that
he or she has a problem. In many cases, it takes a significant event -- such as
the loss of a job, the break-up of a marriage, an arrest, or health crisis -- to force the addict to admit to his or her problem.
Treatment of sexual addiction focuses on controlling the addictive behavior and helping the person develop a healthy sexuality. Treatment includes education about healthy sexuality, individual counseling, and marital and/or family therapy. Support groups and 12 step recovery programs for people with sexual addictions (like Sex Addicts Anonymous) also are available. In some cases, medications used to treat obessesive compulsive disorder may be used to curb the compulsive nature of the sex addiction. These drugs could include prozac and anafril
Sex addicts engage in distorted thinking, often rationalizing and justifying their behavior and blaming others for problems. They generally deny they have a problem and make excuses for their actions.
Sexual addiction also is associated with risk-taking. A person with a sex addiction engages in various forms of sexual activity, despite the potential for negative and/or dangerous consequences. In addition to damaging the addict's relationships and interfering with his or her work and social life, a sexual addiction also puts the person at risk for emotional and physical injury.
For some people, the sex addiction progresses to involve illegal activities, such as exibitionism (exposing oneself in public), making obscene phone calls, or molestation. However, it should be noted that sex addicts do not necessarily become sex offenders.
Behaviors associated with sexual addiction include:
- Compulsive masterbation (self-stimulation)
- Multiple affairs (extra-marital affairs)
- Multiple or anonymous sexual partners and/or one-night stands
- Consistent use of pornography
- Unsafe sex
- Phone or computer sex (cybersex)
- Prostitution or use of prostitutes
- Exhibitionism
- Obsessive dating through personal ads
- Voyeruism (watching others) and/or stalking
- Sexual harassment
- Molestation /rape
How is sexual addiction treated?
Treatment of sexual addiction focuses on controlling the addictive behavior and helping the person develop a healthy sexuality. Treatment includes education about healthy sexuality, individual counseling, and marital and/or family therapy. Support groups and 12 step recovery programs for people with sexual addictions (like Sex Addicts Anonymous) also are available. In some cases, medications used to treat obessesive compulsive disorder may be used to curb the compulsive nature of the sex addiction. These drugs could include prozac and anafril
FEMALE SEXUAL DYSFUNCTION TREATMENT
Sexual dysfunction includes desire, arousal, orgasmic and sex pain
disorders (dyspareunia and vaginismus). Primary care physicians must
assume a proactive role in the diagnosis and treatment of these
disorders. Long-term medical diseases, minor ailments, medications and
psychosocial difficulties, including prior physical or sexual abuse, are
etiologic factors. Gynecologic maladies and cancers (including breast
cancer) are also frequent sources of sexual dysfunction. Patient
education and reassurance, with early diagnosis and intervention, are
essential for effective treatment. Patient history and physical
examination techniques, normal sexual responses and the factors that
influence these responses, and the application of medical and
gynecologic treatments to sexual issues are discussed. Basic treatment
strategies, which may be successfully provided by primary care
physicians for most sexual dysfunctions, are outlined. Referral can be
reserved for patients who do not respond to therapy.
Sexuality is a complex process, coordinated by the neurologic, vascular and endocrine systems. Individually, sexuality incorporates family, societal and religious
beliefs, and is altered with aging, health status and personal
experience. In addition, sexual activity incorporates interpersonal
relationships, each partner bringing unique attitudes, needs and
responses into the coupling. A breakdown in any of these areas may lead
to sexual dysfunction.Primary care physicians, skilled in the treatment of medical and psychologic disorders, often feel unqualified to treat patients with sexual dysfunction. However, with an understanding of sexual functioning and application of general medical and gynecologic treatments to sexual issues, sexual dysfunction may be effectively approached with the same skills. The latter includes obtaining a complete patient history, conducting a physical examination, application of basic treatment strategies, providing patient education and reassurance, and recommending appropriate referral when indicated.
Diagnosis
Female sexual dysfunction can be subdivided into desire, arousal, orgasmic and sexual pain disorders. Sexual pain disorders include dyspareunia and vaginismus.Estimates of the number of women who have sexual dysfunction range from 19 to 50 percent in “normal” outpatient populations and increase to 68 to 75 percent when sexual dissatisfaction or problems (not dysfunctional in nature) are included. Yet, one review of physicians' chart notes revealed a recorded sexual problem in only 2 percent. In another review, physician inquiry of patients in a gynecologic office setting about sexual problems increased reported complaints about sexual dysfunction sixfold. This discrepancy demonstrates a need for physician education in this area.
The diagnosis of female sexual dysfunction requires the physician to obtain a detailed patient history that defines the dysfunction, identifies causative or confounding medical or gynecologic conditions, and elicits psychosocial information.Preappointment questionnaires or appointments at which only the history is taken allow patient-physician communication to be unhindered by time constraints or patient fears of an upcoming physical examination.
Establishment of the patient's sexual orientation is necessary for appropriate evaluation and management. Nonjudgmental, direct questions best achieve this goal. Because gender identity conflicts are often a cause of sexual dysfunction, the mode and type of questions asked by physicians should create an environment where patients may openly express their concerns. Specialized counseling is important for these patients.
The sexual dysfunction should be defined in terms of onset and duration and situational versus global effect. A situational dysfunction occurs with a specific partner, in a certain setting or in a definable circumstance.
The presence of more than one dysfunction should be ascertained, because considerable interdependence may exist. For example, a patient complaining about decreased desire might have a primary orgasmic disorder from insufficient stimulation, with decreased desire developing secondarily as a result of unsatisfying sexual encounters (Thus, treating the orgasmic disorder would indirectly enhance desire; whereas, treating a desire disorder would be unsuccessful and perhaps add to patient frustration and perpetuate the cycle of dysfunction.

FIGURE 1.
Cycle
of sexual dysfunction. Example showing how a patient can enter the
cycle of sexual dysfunction in one area (i.e., decreased orgasm) and
proceed to another area (i.e., decreased desire) so that the presenting
complaint may not represent the problem that actually requires
evaluation and treatment.
Adapted with permission from Phillips NA. The clinical evaluation of dyspareunia. Int J Impot Res 1998;10(suppl 2):S117–20.
Medical conditions are a frequent source of direct or indirect sexual difficulties. Vascular disease associated with diabetes might preclude adequate arousal; cardiovascular disease may inhibit intercourse secondary to dyspnea Arthritis or urinary incontinence may cause discomfort or embarrassment, leading to dysfunction or decreased sexual activity.Aggressive treatment of long-term disease and minor ailments, with attention to their sexual implications, will help enhance sexuality.
Medical Causes of Female Sexual Dysfunction
Prescription and over-the-counter medications, illicit drugs and alcohol abuse contribute to sexual dysfunction
Medication changes, drug discontinuation, or dosage or schedule
alterations may provide relief. Cigarette smoking, known to cause
erectile dysfunction in men, may have a similar negative effect on
arousal in women.
The
rightsholder did not grant rights to reproduce this item in electronic
media. For the missing item, see the original print version of this
publication.
Medications and Female Sexual Dysfunction
Medications that cause disorders of desire
| |
Psychoactive medications
| |
Antipsychotics
| |
Barbiturates
| |
Benzodiazepines
| |
Selective serotonin reuptake inhibitors
| |
Lithium
| |
Tricyclic antidepressants
| |
Cardiovascular and antihypertensive medications
| |
Antilipid medications
| |
Beta blockers
| |
Clonidine (Catapres)
| |
Digoxin
| |
Spironolactone (Aldactone)
| |
Hormonal preparations
| |
Danazol (Danocrine)
| |
GnRh agonists (e.g., Lupron, Synarel)
| |
Oral contraceptives
| |
Other
| |
Histamine H2-receptor blockers and promotility agents
| |
Indomethacin (Indocin)
| |
Ketoconazole (Nizoral)
| |
Phenytoin sodium (Dilantin)
| |
Medications that cause disorders of arousal
| |
Anticholinergics
| |
Antihistamines
| |
Antihypertensives
| |
Psychoactive medications
| |
Benzodiazepines
| |
Selective serotonin reuptake inhibitors
| |
Monoamine oxidase inhibitors
| |
Tricyclic antidepressants
| |
Medications that cause orgasmic dysfunction
| |
Methyldopa (Aldomet)
| |
Amphetamines and related anorexic drugs
| |
Antipsychotics
| |
Benzodiazepines
| |
Selective serotonin reuptake inhibitors
| |
Narcotics
| |
Trazadone (Desyrel)
| |
Tricyclic antidepressants*
| |
*—Also associated with painful orgasm
Adapted with permission from Drugs that cause sexual dysfunction: an update. Med Lett Drugs Ther 1992;34:73–8.
Gynecologic Causes of Female Sexual Dysfunction and Method of Gynecologic Examination
| Examination | Condition |
|---|---|
External genitalia
| |
Assess muscle tone
|
Vaginismus
|
Assess skin color and texture
|
Vulvar dystrophy, dermatitis
|
Assess skin turgor and thickness
|
Atrophy
|
Assess pubic hair amount and distribution
|
Atrophy
|
Expose clitoris
|
Clitoral adhesions
|
Assess for ulcers
|
Herpes simplex virus
|
Perform cotton swab test of vestibule
|
Vulvar vestibulitis
|
Palpate Bartholin glands
|
Bartholinitis
|
Assess posterior forchette and hymenal ring
|
Episiotomy scars, strictures
|
Monomanual
|
|
Palpate rectovaginal surface
|
Rectal disease
|
Palpate levator ani
|
Levator ani myalgia, vaginismus
|
Palpate bladder/urethra
|
Urethritis, interstitial cystitis, urinary tract infection
|
Assess for cervical motion tenderness
|
Infection, peritonitis
|
Assess vaginal depth
|
Postoperative changes, postradiation changes, stricture
|
Bimanual
|
|
Palpate uterus
|
Retrogression, fibroids, endometritis
|
Palpate adnexa
|
Masses, cysts, endometriosis, tenderness
|
Perform rectovaginal examination
|
Rule out endometriosis
|
Obtain guaiac test
|
Bowel disease
|
Speculum
|
|
Evaluate discharge, pH
|
Vaginitis, atrophy
|
Evaluate vaginal mucosa
|
Atrophy
|
Perform Papanicolaou smear
|
Human papillomavirus infection, cancer
|
Assess for prolapse
|
Cystocele, rectocele, uterine prolapse
|
Adapted with permission from Phillips NA. The clinical evaluation of dyspareunia. Int J Impot Res 1998;(suppl 2):S117–20.
Gynecologic changes related to a woman's reproductive life (e.g., puberty, pregnancy, the postpartum period and menopause) present unique problems and potential obstacles to sexuality. Puberty may lead to concerns regarding sexual identity. Pregnancy and the postpartum period are often associated with a decrease in sexual activity, desire and satisfaction, which may be prolonged with lactation.
The hypoestrogenic state of menopause may cause significant physical changes and alterations in mood or a diminished sense of well-being, which have been found to have a significant, negative impact on sexuality. A decline in desire, arousal and frequency of intercourse and an increase in dyspareunia have been associated with menopause, although these findings are not universal.
Physiologic Changes of Menopause
Skin
|
Decreased activity of sweat and sebaceous glands, decreased tactile stimulation
|
Breasts
|
Decreased fat content, decreased breast swelling and nipple erectile response with sexual arousal
|
Vagina
|
Shortening
and loss of elasticity of vaginal barrel, diminished physiologic
secretions, rise in vaginal pH from 3.5 to 4.5 to greater than 5,
thinning of epithelial layers
|
Internal reproductive organs
|
Ovaries
and fallopian tubes diminish in size, ovarian follicles undergo
atresia, ovarian stroma becomes fibrotic, uterine body weight decreases
30 to 50 percent, cervix atrophies and decreases mucous production
|
Bladder
|
Urethra and bladder trigone atrophy
|
Reproduced
with permission from Phillips NA, Rosen RC. Menopause and sexuality.
In: Lobo RA, ed. Treatment of the postmenopausal woman. 2d ed.
Phildelphia: Lippincott Williams and Wilkins, 1999:437–43.
Psychosocial Factors of Female Sexual Dysfunction
Intrapersonal conflicts
|
Religious taboos, social restrictions, sexual identity conflicts, guilt (i.e., widow with new partner)
|
Historical factors
|
Past or current abuse (sexual, verbal, physical), rape, sexual inexperience
|
Interpersonal conflicts
|
Relationship
conflicts; extra-marital affairs; current physical, verbal or sexual
abuse; sexual libido; desire or practices different from partner; poor
sexual communication
|
Life stressors
|
Financial, family or job problems, family illness or death, depression
|
PHYSICAL EXAMINATION
Each patient should
undergo a thorough examination, with the gynecologic examination
individually guided by and tailored to patient comfort. The goal of the
examination is detection of disease; however, the examination also
provides an opportunity to educate the patient about normal anatomy and
sexual function, and to reproduce and localize pain encountered during
sexual activity.A routine examination seeks signs of general medical conditions. The gynecologic examination is comprehensive beginning with inspection of the external genitalia, including a cotton swab test if indicated (gently touching the vestibule of the vagina with a cotton swab will elicit moderate to severe pain in patients with vulvar vestibulitis). For patients with dyspareunia, a “mono-manual” examination should follow, with one or two fingers in the vagina (proceeding from posterior to anterior), and the other hand held away from the abdomen so as not to confuse the source of discomfort Bimanual and rectovaginal examinations are then performed. The timing of the speculum examination is guided by patient symptoms. In patients with deep dyspareunia, the speculum examination should follow the bimanual examination because localization of pain is crucial in these patients. In patients in whom vaginitis, cervical cancer or a sexually transmitted disease is suspected, cultures and vaginal samples should be obtained first.
Laboratory testing should be guided by patient symptoms and examination findings. No specific tests are universally recommended for patients with sexual dysfunction. Attention to routine screening tests must not be overlooked.
General Treatment Guidelines
Following the patient history and physical examination, a suspected etiology may be treated.If no etiology is discovered, basic treatment strategies are applied The patient's (and partner's) personal tastes and comfort must be considered. Physicians should respect a patient's choice to decline treatment, because studies show that sexual activity is not correlated with overall sexual satisfaction or intimacy in all persons. In general, treatments are similar despite sexual orientations.
Basic Treatment Strategies for Female Sexual Dysfunction
Provide education
|
Provide
information and education (e.g., about normal anatomy, sexual function,
normal changes of aging, pregnancy, menopause). Provide booklets,
encourage reading; discuss sexual issues when a medical condition is
diagnosed, a new medication is started, and during pre- and
postoperative periods; give permission for sexual experimentation.
|
Enhance stimulation and eliminate routine
|
Encourage
use of erotic materials (videos, books); suggest masturbation to
maximize familiarity with pleasurable sensations; encourage
communication during sexual activity; recommend use of vibrators*;
discuss varying positions, times of day or places; suggest making a
“date” for sexual activity.
|
Provide distraction techniques†
|
Encourage
erotic or nonerotic fantasy; recommend pelvic muscle contraction and
relaxation (similar to Kegel exercise) exercises with intercourse;
recommend use of background music, videos or television.
|
Encourage noncoital behaviors‡
|
Recommend
sensual massage, sensate-focus exercises (sensual massage with no
involvement of sexual areas, where one partner provides the massage and
the receiving partner provides feedback as to what feels good; aimed to
promote comfort and communication between partners); oral or noncoital
stimulation, with or without orgasm.
|
Minimize dyspareunia
|
Superficial: female astride for control of penetration, topical lidocaine, warm baths before intercourse, biofeedback.
|
Vaginal: same as for superficial dyspareunia but with the addition of lubricants.
|
Deep:
position changes so that force is away from pain and deep thrusts are
minimized, nonsteroidal anti-inflammatory drugs before intercourse.
|
note: For a review, see Striar S, Bartlik B. Stimulation of the libido: the use of erotica in sex therapy. Psych Annals 1999;29:60–2.
—Provide information for obtaining one discreetly.
—Helpful in eliminating anxiety, increasing relaxation and diminishing spectatoring.
—Also helpful if partner has erectile dysfunction.
DISORDERS OF DESIRE
Women with disorders of
desire are difficult to treat. Occasionally, decreased desire in
patients is secondary to boredom with sexual routines. Suggesting
changes in positions or venues, or the addition of erotic materials is
helpful.Disorders of desire in premenopausal patients may be secondary to lifestyle factors (e.g., careers, children), medications or another sexual dysfunction (e.g., pain or orgasmic disorder). No medical treatment is available specific to patients with disorders of desire. If no underlying medical or hormonal etiology is discovered, individual or couple counseling may be helpful.
In peri- and postmenopausal women, the relationship between hormones and sexuality is unclear. Nonetheless, estrogen replacement therapy has been shown to correlate positively with sexual activity, enjoyment and fantasies—the latter thought to represent desire. The mechanism of estrogen's effect on desire is indirect and occurs through improvement in urogenital atrophy, vasomotor symptoms and menopausal mood disorders (i.e., depression). This relationship helps predict which patients are likely to respond to estrogen replacement therapy (i.e., those with symptoms of hypoestrogenism) and may explain why some studies do not show estrogen-mediated improvement in sexual functioning.
The role of progesterone therapy, which is necessary in estrogen-treated patients with an intact uterus, has not been widely studied in terms of sexuality, but one study suggests that it exhibits a negative impact by dampening mood and decreasing available androgens. The addition of estrogen for several weeks before progesterone therapy is initiated, or taking into account monthly symptom calendars, will help determine each hormone's influence and guide dosage and schedule adjustments.
Testosterone appears to have a direct role in sexual desire. However, because studies evaluate mostly testosterone-deficient, oophorectomized women or women who develop supraphysiologic levels secondary to testosterone treatment, clinical applications are limited. No guidelines for testosterone replacement therapy for women with disorders of desire and no consensus of “normal” or “therapeutic” levels of testosterone therapy exist. Many physicians are concerned about the lack of safety data on the role of testosterone in breast cancer and on hepatic side effects; however, hepatocellular damage or carcinoma is rare at prescribed dosages, and the development of breast cancer has not been reported clinically.
The side effects of testosterone, which occur in 5 to 35 percent of patients, include lower levels of high-density lipoprotein, acne, hirsutism, clitorimegaly and voice deepening. However, these side effects on lipoprotein levels are rarely significant if estrogen and testosterone are coadministered; moreover, most other side effects are reversible with discontinuation of testosterone or a dosage adjustment.
A role for testosterone treatment exists in selected patients . Coadministration with estrogen therapy should be provided to prevent deleterious effects on lipoprotein levels. Before initiating testosterone treatment, physicians should discuss the potential and theoretic risks, and individual risk and benefit assessments with the patient. In general, patients with current or previous breast cancer, uncontrolled hyperlipidemia, liver disease, acne or hirsutism should not receive testosterone therapy.
Testosterone Therapy for Treatment of Disorders of Desire
Screening
|
Baseline
testosterone levels† (free and total), baseline lipid profile, baseline
liver enzyme levels, mammography, Papanicolaou smear
|
Initiate therapy‡
|
Combination product (Estratest or Estratest hs)
|
Methyltestosterone (Android), 1.25 to 2.5 mg daily
|
Micronized oral testosterone, 5 mg twice daily
|
Testosterone proprionate 2 percent in petroleum applied daily to every other day
|
Testosterone injectables/pellets
|
Reevaluation at three to four months
|
Repeat testosterone levels, lipid profile, liver enzyme levels
|
Monitor symptoms, side effects
|
Continued therapy
|
Taper to lowest effective dosage
|
Monitor lipid levels, liver enzyme levels once or twice yearly
|
Routine Papanicolaou smear and mammography schedules
|
—These
are recommendations; no evidence-based protocols are available on
testosterone therapy for the treatment of women with desire disorders.
—Many authors recommend that total levels remain in “normal” range for pre-menopausal women.
—None of these medications are labeled by the U.S. Food and Drug Administration for treatment of desire disorders.
—Alternate
daily combined with estrogen-only pill, take testosterone pill every
other day, 5 days a week, etc. (not shown in studies to be safer or have
fewer side effects).
AROUSAL DISORDERS
Current treatment of
patients with arousal disorders is limited to the use of commercial
lubricants, although vitamin E and mineral oils are also options.
Arousal disorders may be secondary to inadequate stimulation, especially
in older women who require more stimulation to reach a level of arousal
that was more easily attained at a younger age. Encouraging adequate
foreplay or the use of vibrators to increase stimulation may be helpful.
Taking a warm bath before intercourse may also increase arousal.
Anxiety may inhibit arousal, and strategies to alleviate anxiety by
employing distraction techniques are helpful.Urogenital atrophy is the most common cause of arousal disorders in postmenopausal women, and estrogen replacement, when appropriate, is usually effective therapy. However, women taking systemic estrogens occasionally require supplementation with local therapy. Long-term use of estrogen-containing vaginal creams is considered an unopposed-estrogen treatment in women with an intact uterus, requiring progesterone opposition. An oral progesterone such as medroxyprogesterone 5 mg daily for 10 days every one to three months (or equivalent) may be used initially, with frequency or dosage increased if withdrawal bleeding occurs. Estring (an estradiol-containing vaginal ring) has little systemic absorption and does not require the addition of progesterone. Patients who are uncomfortable wearing the ring during the day often achieve relief with night use only.
Premenopausal women with arousal disorders, women who do not respond to estrogen therapy and women who are unable or unwilling to take estrogen represent difficult patient groups because few treatment options are available.
Investigators recognize that small-vessel atherosclerotic disease of the vagina and clitoris may contribute to arousal disorders and are exploring vasoactive medications as treatment. Small studies have been conducted with favorable results, but larger studies are needed. Currently, treatment of arousal disorder in women who are taking these medications, including sildenafil (Viagra), is not recommended, although anecdotal success has been reported.
ORGASMIC DISORDERS
Anorgasmia is quite
responsive to therapy. This condition is caused by sexual inexperience
or the lack of sufficient stimulation and is common in women who have
never experienced orgasm. Orgasmic disorders may also be psychologic
(“involuntary inhibition” of the orgasmic reflex) or caused by
medications or chronic disease.Treatment relies on maximizing stimulation and minimizing inhibition. Stimulation may include masturbation with prolonged stimulation (initially up to one hour) and/or the use of a vibrator as needed, and muscular control of sexual tension (alternating contraction and relaxation of the pelvic muscles during high sexual arousal). The latter is similar to Kegel exercises . Methods to minimize inhibition include distraction by “spectatoring” (observing oneself from a third-party perspective), fantasizing or listening to music. Women who do not respond to therapy should be referred to an appropriate therapist.
Kegel Exercises
Potential uses
|
Increased pubococcygeal tone
|
Improved orgasmic intensity
|
Correction of orgasmic urine leakage
|
Distraction technique during intercourse
|
Improved patient awareness of sexual response
|
Teaching Kegel exercises
|
Instructional examination with examiner's finger in vagina
|
Initial patient home exercise with patient's finger in vagina
|
Slow count to 10, with movement directed “in and up”
|
Hold for count of 3
|
Slow release to count of 10
|
Repeat 10 to 15 times daily
|
Consider vaginal weights, biofeedback clinics
|
Maintaining Kegel exercises
|
Advise repetitions during routine activities (standing in line, at stop lights, etc.)
|
Schedule follow-up appointments to discuss progress
|
SEX PAIN DISORDERS
Dyspareunia can be divided into three types of pain: superficial, vaginal and deep .
Superficial dyspareunia occurs with attempted penetration, usually
secondary to anatomic or irritative conditions, or vaginismus. Vaginal
dyspareunia is pain related to friction (i.e., lubrication problems),
including arousal disorders. Deep dyspareunia is pain related to
thrusting, often associated with pelvic disease or relaxation.Diagnosis of an underlying etiology should be aggressively sought, even if surgical investigation (laparoscopy) is required. The physical examination must include meticulous detail, with the physician's focus on recreating the pain. Treatment of the underlying etiology is fundamental, but as in long-term pain disorders, counseling and pain control strategies are essential. General recommendations for improved sexual function are discussed in and are similar despite sexual orientation.
Vaginismus, the involuntary contraction of the muscles of the outer one third of the vagina, is often related to sexual phobias or past abuse or trauma. Vaginismus may be complete or situational, so that a pelvic examination might be possible while intercourse is not. Therapy for and counseling of women with vaginismus can be initiated and often successfully completed by primary care physicians.
Treatment of women with vaginismus consists of progressive muscle relaxation and vaginal dilatation (actually a misnomer because the vagina is not physically stretched). Progressive muscle relaxation can be taught during an instructional examination by having the patient alternate contracting and relaxing the pelvic muscles around the examiner's finger. Women with vaginismus can achieve vaginal dilatation with the use of commercial dilators or tampons of increasing diameter, placed into the vagina for 15 minutes twice daily. Once the patient can easily accept an equivalent-sized dilator into the vagina, penile penetration by the partner can occur. Success rates approach 90 percent. Patients who do not respond to this therapy should be referred to a sex therapist who specializes in the treatment of women with this disorder .
Female Sexual Dysfunction: When to Refer
Longstanding dysfunction
|
Multiple dysfunctions
|
Current or past abuse
|
Psychologic disorder or acute psychologic event Unknown etiology
|
No response to therapy
|
Subscribe to:
Posts (Atom)